Nonoperative Treatments
MEDICATIONS
There currently are no FDA approved medications to treat cartilage conditions. Some studies have demonstrated that the use of the nutritional supplement glucosamine might slow the destructive changes that occur in articular cartilage. Medications labelled as arthritis medicine target the pain and symptoms such as swelling and stiffness that are associated with osteoarthritis. Patients and their doctors should work collaboratively to determine the most effective medication to relieve those symptoms while causing the least side effects. Options include pain relievers such as acetaminophen , ibuprofen, naproxen, or prescription nonsteroidal anti-inflammatory drugs.
WEIGHT LOSS
Carrying extra weight has been shown to exert a greater demand on the joint and can lead to a greater deterioration and progression of knee arthritis. This often results in a very cyclic pattern. Activity decreases as the result of the pain, stiffness, and swelling experienced in the joint and the reduction in activity often leads to even more weight gain and more stress and strain on the joints. Measures should be taken to find an exercise regimen that will promote activity and weight loss without triggering the pain associated with high impact exercise. Restoring strength and flexibility in the muscles from the back and pelvis through the entire leg can assist in reducing the workload directly on the knee/joint.
LOCAL PAIN MANAGEMENT
Cold therapy is often used in the early stage of an injury to decrease the associated swelling and pain. Heat therapy is often used in later or more chronic phases of knee problems to increase the blood flow and diminish stiffness and pain.
INJECTIONS: CORTICOSTEROIDS AND VISCOSUPPLEMENTS
Cortisone injections have been used for many, many years to reduce knee pain.
Viscosupplementation involves injecting a preparation of hyaluronic acid into the knee joint to improve the activity of the knee and to diminish the pain experienced at rest.
ELECTRICAL STIMULATION
The use of pulsed electrical signals to the knee to improve pain and function of the extremity.
BRACING
There are several bracing options that are available to manage the pain, stiffness, and swelling associated with knee cartilage conditions. An unloader brace transfers a portion of the load/weight to the unaffected side of the joint. Other braces are designed to help control abnormal movements of the knee.
THERAPY
The knee experiences a very high workload just from the activities of daily living alone. The muscles of the knee serve as shock absorbers for the joint and an exercise regimen designed by a physical therapist targeting the muscles that serve the back, pelvis, hip, and knee are important to build strength and prevent further damage or pain.
Operative Treatments: Surgical Repair
MENISCAL REPAIR
The meniscus cartilage tissue between the thigh/femur and the shin/tibia is frequently torn during strenuous activity at work or while engaging in sports. Only a small portion of meniscal tears are in a location with an adequate blood supply (10%). To be “repaired” a tear must be near an adequate blood supply.
Meniscal tears can be repaired using a variety of techniques ranging from very basic suture repairs through complex arthroscopic procedures.
ARTICULAR CARTILAGE REPAIR
It is believed that the articular cartilage (that which covers the bones at the joint) cannot be repaired and, at best, a surgeon can only re-implant cartilage that has been dislodged.
LIGAMENT REPAIR
Surgical repair is limited to ligaments that heal better with surgery. The medial collateral ligament (MCL) has a robust blood supply so can typically repair itself without surgical intervention. The anterior collateral ligament (ACL) does not have that same good blood supply and is seated deep within the knee joint so typically does not repair itself with or without surgical intervention. The patellar tendon is responsible for maintaining the position of the knee cap. If a patella dislocates or is dislodged, the ligament securing it is torn. The patellar tendon may heal on its own or might require surgical repair.
Operative Treatments: Surgical Restoration
MENISCAL RESTORATION
The goal of meniscal surgery is to maintain the cartilage function. Preserving meniscal functionality is a top priority but nearly 90% of tears cannot be repaired so the torn portion is surgically removed. Although this falls into the category of only a partial meniscectomy, the outcome is still the same and from a functional perspective, it results in the same outcome as a total meniscectomy. Arthritis often results over time. Meniscal transplantation involves the use of a size-matched cadaver donor meniscus that is transplanted into the site of the original meniscus with the intent of regaining meniscal function.
ARTHROSCOPIC CHONDROPLASTY AND MICROFRACTURE
For patients who have had the meniscus removed, the surgeon may offer an innovative solution called a meniscal transplant. It is important to remember that even though only a part of the meniscus was removed, at times the effect to the knee from a biomechanical standpoint is the same as a total menisectomy. The indications for transplant need to be assessed by your cartilage surgeon. Unlike other forms of tissue transplantation, this procedure does not require patients to be on medications to prevent rejection. Intermediate term follow-up studies in the literature are encouraging.
ARTICULAR RESTORATION
The articular cartilage that covers the bones at the joint experiences a constant wear and tear. The cells of the articular cartilage, called the chondrocytes, make the matrix or this external covering of the bones. Chondrocytes do not replicate, cannot repair themselves when injured, and also decrease in number as the aging process progresses. The damaged or lost chondrocytes then fail to support the articular cartilage regeneration process and articular cartilage defects occur. Articular restoration procedures either enable the surgeon to stimulate a healing response or replace the worn tissue completely.
OSTEOCHONDRAL AUTOGRAFT (OATS)
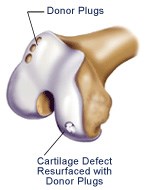
This technique is analogous to a hair-plug transfer. The surgeon removes a small section of the patient’s own cartilage along with the underlying bone plug. This is obtained from an area which does not participate in high loading.
This bone and cartilage (hence osteo—chondral) local graft is then transferred to the defect where a receiving hole has been prepared. Obviously, there is a limit to the amount of tissue available for “harvesting.” The typical site of harvest is at the margin of the femoral trochlea where the patella glides—if that area is involved with damage then this technique may not be possible. The size of the defect treatable with this method is usually between 1 and 2 square cm or slightly larger than a thumbnail.
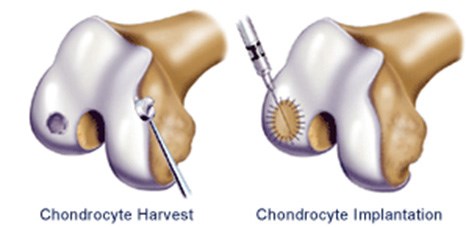
AUTOLOGOUS CARTILAGE CELL IMPLANTATION
For articular cartilage defects greater than 2cm2, one of the more advanced techniques for cartilage regeneration is ACI (Autologous Chondrocyte Implantation).
The first stage may be performed when initially assessing the joint arthroscopically. A small amount of the patient’s own articular cartilage is harvested. Through cell culturing techniques, the cell number is increased from a few hundred thousand to over 10 million cells. These autologous (your own) cultured cells are then implanted in the knee in a second surgical procedure to repair and resurface areas of cartilage loss. The cells (the marshmallows) represent only 1-5% of the volume of the matrix (jello). These cells must synthesize (create) matrix over several months to reestablish the articular surface.
LIGAMENT RESTORATION
Ligaments connect bones and stabilize their position. Loss of ligament function results in instability. The instability causes multiple problems including loss of functionality as well as an abnormal stress load on the cartilage, furthering the damage. Ligaments that do not heal may require reconstruction. The most recognized sports-related ligament reconstruction is anterior cruciate ligament reconstruction (ACL reconstruction) to prevent lateral direction change knee instability. The goal for the surgical intervention is always to reproduce the natural ligament function to the extent possible.
Operative Treatments: Osteotomies
HIGH TIBIAL OSTEOTOMY (HTO)
HTO is an osteotomy procedure for bowlegged patients. The tibia (shin) is cut and straightened out, then held in place with a plate and screws. It is performed for localized arthritis on the inside part of the knee.
DISTAL FEMORAL OSTEOTOMY (DFO)
Similar to the HTO, but used for the treatment of knock-kneed patients with arthritis of the lateral (outside) part of the knee. Here, the femur (thighbone) is cut and straightened.
TIBIAL TUBERCLE OSTEOTOMY (TTO)
The procedure is useful for the treatment of patellar dislocations as well as for specific areas of arthritis behind the kneecap.
Operative Treatments: Replacement Alternatives
UNICOMPARTMENTAL KNEE REPLACEMENT (PARTIAL KNEE REPLACEMENT)
The knee joint is comprised of three distinct compartments. It is not uncommon for one side of the knee or the other to experience wear from osteoarthritis while the remainder of the knee is unaffected. In this scenario, rather than replacing the entire knee (both good and bad compartments), it is possible to least invasive to replace only the single side impacted by the arthritis.
PATELLOFEMORAL KNEE REPLACEMENT
The third section of the knee is the kneecap and the section in which it glides—the Patellofemoral compartment. A small number of patients will have arthritis only in this segment of the knee. This section only can be replaced in what is known as a patellofemaoral joint replacement which allows the ligaments of the knee and the other two regions to be completely preserved. The motion of the knee is more natural when only this compartment is replaced.
BICOMPARTMENTAL KNEE REPLACEMENT
In certain instances two of the three compartments of the knee are impacted by arthritis and a bicompartmental knee replacement targets only two segments rather than all three. This is favorable because it spares two of the four ligaments' complexes located within the knee.
